Healthcare Professionals' Experiences and Perspectives on Disclosure of Misattributed Parentage in Clinical Settings
Leah Westcott
Co-Presenters: Individual Presentation
College: The College of Health Professions and Human Services
Major: Genetic Counseling
Faculty Research Mentor: Laura Limone
Abstract:
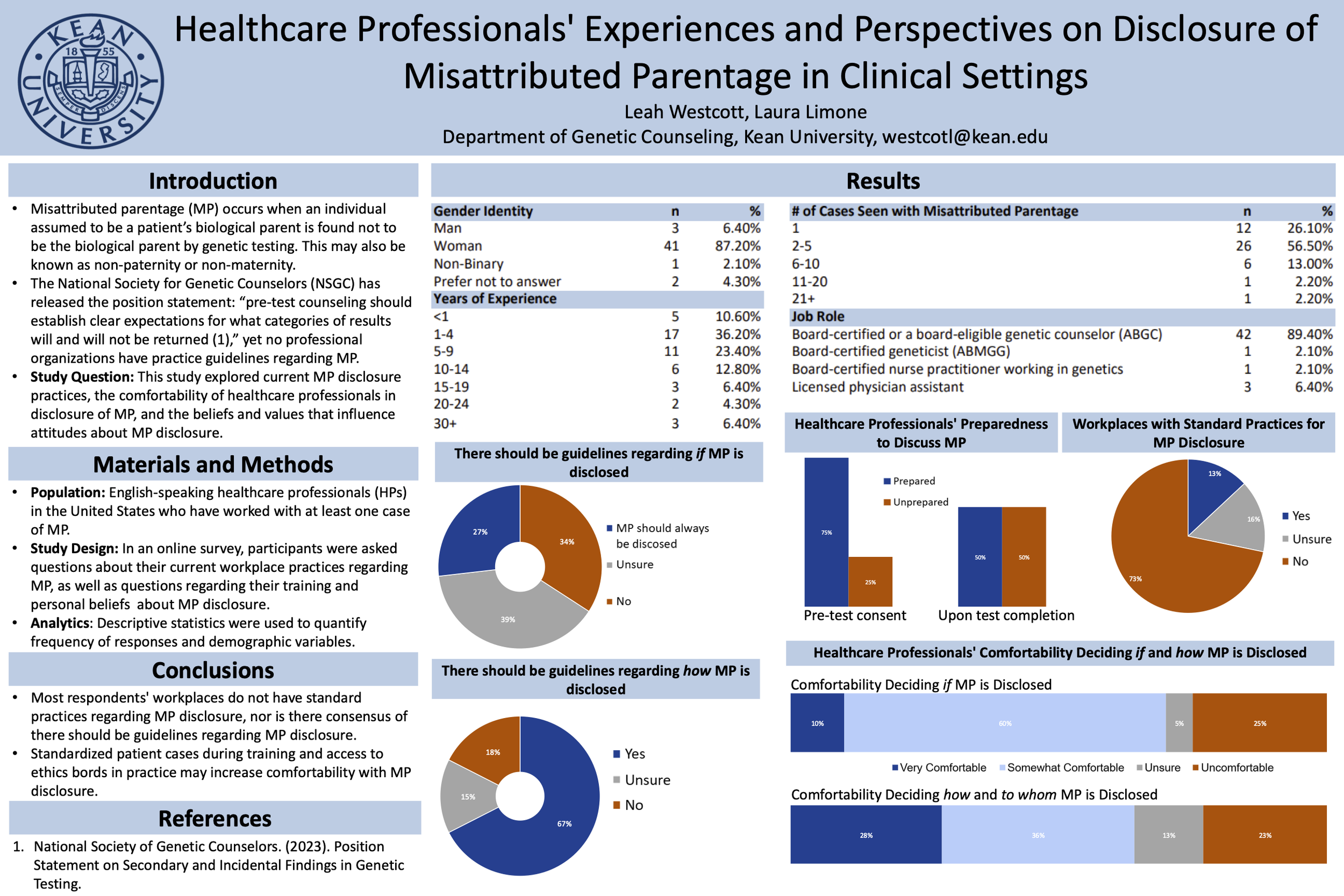
Introduction: Misattributed parentage (MP) occurs when a presumed biological parent is not the genetic parent, encompassing both non-paternity and non-maternity. Advances in genetic testing have improved MP detection, resulting in more unexpected findings. The decision to disclose MP is typically made by genetics professionals, yet no standardized protocols exist, creating ethical challenges in non-disclosure or selective disclosure. As genetic testing becomes more common, the detection of MP is expected to rise, emphasizing the need for clear guidelines on informed consent, disclosure practices, and comprehensive training for healthcare professionals involved in genetic testing.Purpose: This study explored how healthcare professionals handle MP findings, their training and practices for disclosure, and the values and beliefs that inform their decision-making processes.Methods: Healthcare professionals who encountered at least one case MP were recruited via email blasts, social media, and chain sampling. Participants completed an anonymous online survey, created with Qualtrics. The survey gathered quantitative data on MP disclosure practices, beliefs, and training. Data was analyzed using SPSS, specifically using paired t-tests and linear regressions.Conclusion: Of the 46 survey respondents, 41 (89.13%) were genetic counselors, mostly in pediatric settings. A lack of standardized guidelines was apparent, with 71% reporting no clear procedures for MP disclosure and 17% unsure. Most respondents felt somewhat comfortable with MP disclosure decisions (33%) and to whom it is disclosed (57%). Comfortability did not differ by years in practice (p=0.376), but those with more MP cases felt more comfortable deciding whether to disclose (p=0.028). Opinions on industry guidelines were mixed: 27.5% favored mandatory disclosure, 35% opposed guidelines, and 37.5% were unsure.Significance: The results highlight the need for healthcare professionals to familiarize themselves with clinic MP disclosure guidelines, or lack thereof. While there is no consensus on standardized practices, genetics training programs should incorporate case examples and standardized patients to prepare trainees for ethical situations before entering the workforce.
Keywords: Genetic Testing, Counseling, Non-Paternity, Ethics, Disclosure